Osteoporosis
Explore Our Approach
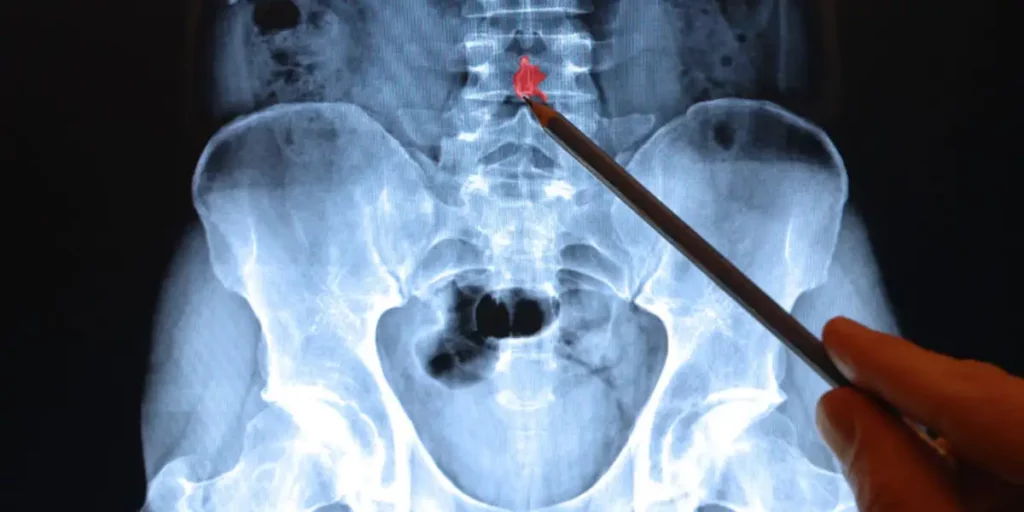
What Is Osteoporosis?
Osteoporosis weakens bone structure, increasing fracture risk. It can be primary or secondary — caused by factors like certain medications (SSRIs, PPIs, corticosteroids, anticoagulants), endocrine disorders, or chronic illness.

First let’s look at what normal bone looks like and how vertebral (irregular) bones are different than long (stick) bones.
Normal Bone Anatomy
Most people think of fractures in terms of long bones, where a bending force snaps the shaft like a stick.
Vertebrae are different: as irregular bones, they fail more often under axial compression or complex loading, crushing rather than snapping.
Their trabecular structure, thin cortical shell, and dense ligamentous and disc attachments distribute forces differently than the solid, elongated shafts of long bones, leading to distinct fracture patterns and biomechanics.
All bones, including long, flat and irregular bones like the vertebrae have common characteristics as well as significant differences.
All bones have distinct components–the dense outer shell known as the cortex and the inner, more hollow, trabecular bone that houses the bone marrow.
The cortex is the outer shell of the bone that’s super hard and dense.
Healthy “cortical” bone has minerals and strong connective tissue built from a base of collagen fibers that gives it most of it’s tensile strength.
Long bones have way more of the outer shell compared to the inner trabecular bone marrow.
Fractures of the cortex in long bones are easy to see on x-rays because the fracture is in the dense, mineralized outer cortex of bone.
They are also painful because it takes a significant structural disruption from trauma to cause it and usually in the arms and legs that are associated with weight bearing.
In contrast, trabecular marrow fractures take less trauma and break at much lower forces than cortical bone.
In fact, trabecular fractures occur constantly all the time and we don’t even notice it.
That’s because most of these fractures are microscopic and occur in normal everyday activities.
It’s a normal part of bone physiology. And this is what is usually occurring in the bones of the vertebrae.
In good bone health, these micro trabecular fractures essentially get healed as fast as we get them–they aren’t healed instantly.
Rather, since there are so many, the body is in a continual balance of healing these fractures.
Bone remodeling occurs continuously in good bone health, with microdamage repair occurring over weeks to months, not instantly.
So the ones healing today are not the ones you got today.
The speed of healing and remodeling slows down with age, certain medications and disease states and allows microdamage accumulation.
As a result, these fractures can accumulate (summation trabecular fractures) and eventually cause pain and even vertebral collapse.
The bone in the marrow is made of microscopic struts that, while strong, are not as strong as the outer cortical bone.

Imagine a skyscraper being built that starts with metal I-beams in a grid/lattice pattern.
The microscopic structure of bone is somewhat similar.
The tiny struts of bone that form the network of microscopic structure of bone are called trabecula or trabeculae (pl)).
While they aren’t straight and and actually form complex interconnections with each other, they can be thought of in simpler terms as the I-beams in bone.
As a result, when they break, the body has to form tiny new blood vessels down them in order to deliver the tools necessary to heal these microscopic fractures.
No new blood vessels or not enough nutrients, and suddenly you start accumulating a bunch of broken struts.
If you think of what would happen in a skyscraper if enough of those metal I-beams were broken in the middle and you can get a picture of the structural damage in osteoporotic bone.
Another way to think of this difference is that the vertebrae of the spine have a much smaller ratio of cortical bone to trabecular bone.
As such, there is proportionally less strong, cortical bone to resist fracture.
In contrast, long bones have a larger cortical bone to trabecular bone ratio meaning that they have more of the dense, tensile strength of cortical bone that helps resist fracture.
Speaking of fracture, long bones and vertebra have other differences.
Biomechanical studies have shown that healthy vertebrae fracture under roughly 3–10 kN of axial compression, while long bone shafts can tolerate much higher bending or torsion forces before reaching the breaking point (Brinckmann et al., Spine, 1988; Burstein et al., J Bone Joint Surg Am, 1972).
In clinical practice, long bone fractures are far more common in trauma because most injury mechanisms apply lever forces to limbs.
In contrast, traumatic vertebral fractures typically require high-energy axial loads like MVAs or fall from a significant height.
Not only can it take less force applied to break a vertebrae compared to a long bone, the forces are typically applied in a different manner.
Also, there are significant differences in stability between these types of bones and their neighbors.
Long bone fractures tend to happen along the stick portion and the forces that cause a fracture are usually either like breaking a stick or a twisting injury (torsion).
Long bones have long stretches of no adjacent bones and their ends tend to be relatively mobile in joints.
How Vertebral Bones Are Different
Spinal Anatomy And Function
In contrast to long bones in the extremities, vertebral fractures tend to occur by an applied compression force down the long axis of the spine or from torsion.
Rather than snapping a stick, vertebral fractures are more like crushing a can or a brick with a hammer.

In addition, the vertebrae as irregular bones tend to be more compact and have many more connections to their neighbors per square inch than long bones.
Each vertebra, for example, has closely applied thick connection tissue connections all around its contact with each adjacent disk.
These anchor the annulus fibrosus of the intervertebral disc to the vertebral endplates.
These tissues, called Sharpey’s fibers, are found in lower concentrations along the shaft (diaphysis) of long bones and mostly function for muscle and ligament attachments.
At the joint ends–in much less density than in the spine.
In addition, large longitudinally oriented ligaments further constrain the spine, connecting vertebrae to each other in front (anterior longitudinal ligament) and back (posterior longitudinal ligament).
Those are just the major stabilizing connective tissues around the cylinder shaped vertebral body.
The remainder and more irregular parts of the vertebral bone are smaller parts that form a ring to protect the spinal cord along with several other smaller bony projections that serve mostly to anchor muscles.
Together these are termed the neural arch and posterior elements.
There are smaller parts of the bone that protrude in various directions for different functions.
Each of these have complex articulations including two paired facet joints, the lateral processes and the spinous processes.

Each of these still has complex, strong connective tissue and ligaments that stabilize these smaller joints.
In addition to the anterior and posterior longitudinal ligaments of the vertebral body, there are even more long ligaments in the posterior elements that further stabilize including the ligamentum flavum, the interspinous ligaments and the supraspinous ligament.
As a unit, along with the disk, these both restrict and allow motion such as bending and twisting in the spine.
Each vertebra carries it’s own weight and the weight of all the ones above it.
The spine carries all of the upper body weight when we are standing and most of it when sitting.
That’s generally about 40% of our total body weight.
As such the spine is continually under greater compressive force than many long bones such as the humerus in the arm.
OLDER REGENERATED Osteoporosis weakens bone structure, increasing fracture risk.
It can be primary or secondary — caused by medications (SSRIs, PPIs, corticosteroids, anticoagulants), endocrine disorders, or chronic illness.
A fragility fracture is, by definition, osteoporosis — regardless of DXA or TBS results.
The Limits of Testing BMD and TBS are valuable but imperfect. They can miss patients with low bone quality who have already had fragility fractures.
Osteoporosis means the bone’s internal structure has weakened, making fractures more likely.
It can be primary (age- or hormone-related) or secondary — due to other conditions or medications.
Secondary osteoporosis can occur even with a normal bone density (BMD) test.
Secondary Causes Include:
- Medications such as SSRIs, proton pump inhibitors (PPIs), corticosteroids, or certain anticoagulants
- Endocrine disorders (thyroid, parathyroid, sex hormone deficiencies)
- Malabsorption syndromes
- Chronic kidney or liver disease
There are many causes of osteoporosis.
In general, once skeletal maturity is achieved in the 20s and growth hormone declines, there is a slow, steady decline in BMD across the rest of our lives.

Theoretically, if you live long enough, you will get age-related osteoporosis from bone loss.
Depending on where you start at skeletal maturity, that might mean you get it at age 63, or you might not get it until 120 years old for example.
Aside from getting older, genetics, medications, hormonal conditions and nutrition are the key factors in developing osteoporosis.
Lifestyle Causes
There are many things in life that can alter our risk for osteoporosis. Decreased mobilization for long periods of time can cause disuse osteoporosis.
This is commonly seen in trauma, prolonged recovery from surgery, or chronic pain syndromes such as those on opioids after failed back surgery.
Gastric bypass surgery, significant weight loss from any cause, anorexia/bulemia and intestinal malabsorption can all cause osteoporosis.

These causes are generally seen as affecting bone quality and the ability of the bone to repair itself due to lack of vitamin D, macronutrients and minerals.
DEXA testing in these patients often lags years behind clinical vertebral fractures.
Medications That Cause Osteoporosis
Many medications can increase our risk for osteoporosis.
Steroids, anti-seizure medications and warfarin are the most well known causes to most doctors, but there are many more that most people do not realize increase their risk.

Steroids:
Getting a steroid dose pack for sinus infections, having your family doctor give you a steroid shot in your hip, taking oral steroids for rheumatoid arthritis or lung disease–these can all cause steroid induced osteoporosis, the prototypical “secondary” osteoporosis.
SSRIs:
Certain antianxiety and antidepressant medications like Prozac can cause osteoporosis in genetically susceptible people.
Often DEXA scans are read as normal in these patients unless a forearm scan is done.
These particular medications are called SSRIs. That stands for selective serotonin reuptake inhibitors.
Many patients are on these for decades and the risk of osteoporosis with these medications increases with time.
Acid Blockers:
Proton pump inhibitors (PPIs) are a class of acid blocking medications that have been associated with secondary osteoporosis.
There is some controversy in the GI doctor literature, but we see this daily.
The misunderstanding seems to be because PPIs generally do not decrease bone mineral density like steroids.
However, the longer a patient has been on PPIs, the higher their risk, particularly for longer than 2 years and over 5 years as well.
While not everyone on PPIs will develop osteoporosis, this is a public health problem because these medications have been given out like candy and are not available over the counter without a prescription.
Not everyone on a PPI will develop osteoporosis, so it seems it’s more likely in patients with certain genetics or other lifestyle factors.
Blood Thinners:
While most physicians are aware that warfarin (Coumadin) causes osteoporosis, I’ve personally seen patients on every class of blood thinner (except aspirin) develop osteoporosis.
Again, not everyone on a blood thinner will develop osteoporosis, but it seems to be a higher percentage of patients than with PPIs.
We aren’t sure of the mechanism yet, but since lifelong anticoagulant therapy is a reality for many patients with heart attack, stroke, and pulmonary embolism, it is a common cause.
Medical Conditions That Cause Osteoporosis
A variety of medical conditions can impact bone health.
Most of these fall in the hormonal, malabsorption and autoimmune categories.
Hormonal Causes of Osteoporosis
- Diabetes
- Thyroid Disorders
- Sex Hormone Disorders
Gut/Malabsorption Causes of Osteoporosis
Most of these causes of osteoporosis reduce the body’s absorption of macronutrients, minerals and fat soluble vitamins in particular (vitamins A, D, E and K).

Vitamin D is the most well established association with impaired bone health as it is a necessary component of bone repair.
Serum vitamin D levels are often a marker of absorption although renal function and sunlight (UV) exposure can affect it as well.
Gastric Bypass
Gastric bypass patients can have functional malabsorption due to surgical changes that affect the ability to take in nutrients in general and fat soluble vitamins in particular.
In addition, they also face the more general osteoporosis risks of significant weight loss which affects the body in numerous ways including macronutrient deficiency.
- Malabsorption
- Crohn’s, Celiac, inflammatory bowel disease
Autoimmune Causes of Osteoporosis
- Lupus
- Others
Genetic Causes of Osteoporosis
- Osteogenesis Imperfecta (OI):
- Ehlers Danlos Syndrome (EDS):
- Non-categorized Familial: Northern European ancestry.
The Limits of BMD & TBS
Bone density scans (DXA) and Trabecular Bone Score (TBS) are valuable, but like all lab tests, they have limitations.
A fragility fracture — a break from a fall at standing height or less — is a disease-defining event for osteoporosis, even if BMD results are normal.
An MSKIR Perspective
Evaluation starts with a thorough history and physical examination.
Diagnosis goes beyond bone density numbers to consider fracture history, metabolic labs, and underlying risk factors.

This comprehensive approach helps guide individualized treatment plans.
The aim is to identify reversible causes and reduce fracture risk.
Treatment Goals
Improve bone strength through medication, nutrition, and exercise – Correct vitamin D deficiency – Address metabolic and hormonal contributors – Prevent future fractures
Request a consultation » Call today! (918) 260-9322
Office Location
Dr. James Webb & Associates, 6550 E 71st St #200, Tulsa, OK 74133
