What is Osteoporosis?
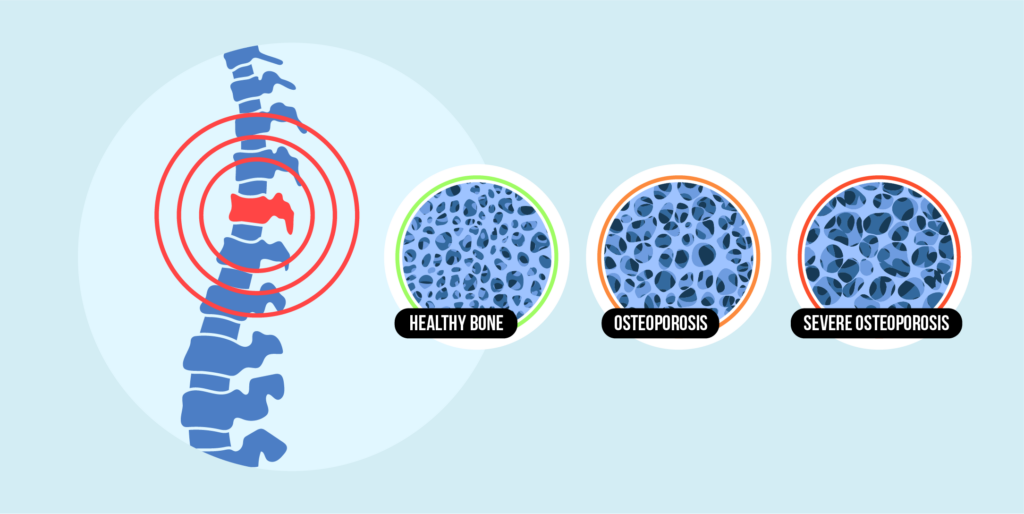
Osteoporosis is a bone disease that is characterized by a decrease in bone mineral density and mass or the change of bone structure and strength.
Such alterations can bring about a decline in bone strength, leading to an increased risk of fractures.

Although called a “silent” disease, osteoporosis tends to develop without obvious symptoms, and many people are not aware of it until bone fracture happens.
Osteoporosis being a condition mostly seen in postmenopausal women and elderly men, is the biggest cause of fractures.
Generally, Bone fractures can make any bone but they occur most commonly in the hip, spinal vertebrae, and in wrist.
How Common is Osteoporosis and Who Gets It?
These Osteoporosis statistics shed light on the wide-ranging impact of osteoporosis, emphasizing the importance of awareness and proactive measures for early intervention and management.

- 50 million Americans are afflicted by osteoporosis.
- Osteoporosis is prevalent in individuals over 50.
- Half of individuals assigned female at birth and 1 in 4 assigned male at birth over 50 have osteoporosis.
- 1 in 3 adults over 50 without osteoporosis display osteopenia.
- Osteoporosis affects individuals of all races and ethnicities.
- Prevalence increases with age, with women often developing the disease before menopause.
- Common among non-Hispanic white and Asian women.
- African American and Hispanic women face lower but significant risks.
- More common in non-Hispanic white men.
What are the Causes of Osteoporosis?
Bone Renewal Process
In young individuals, bone formation exceeds breakdown until around the early 20s, culminating in peak bone mass by 30.
However, as age advances, bone loss outpaces creation, leading to osteoporosis.

Peak Bone Mass
Genetic factors play a role in peak bone mass, varying across ethnicities.
Higher peak bone mass correlates with decreased osteoporosis risk.
Bone Mass Depletion
Osteoporosis ensues when excessive bone mass reduction and structural changes occur, influenced by several risk factors.
Risk Factors
Multiple risk factors influence osteoporosis development, some unmodifiable and others alterable.
Contributing Factors:
Understanding these contributing factors aids in disease and fracture prevention.
- Advanced age: As a person ages, the process of bone growth (also known as bone remodeling) gradually slows down, increasing the risk of osteoporotic fractures after the age of 65.
- Sex: Due to their inherently thinner bones and lesser bone mass than men, women are often more at risk.
- History of fractures: A higher risk of osteoporosis may be indicated by a personal history of broken bones or fragility fractures in maturity (beyond age 45). A parent’s history of osteoporosis or fragility fractures in adulthood, particularly the mother’s, may also increase the risk of developing the condition.
- Genetics: Between the ages of 18 and 25, the bone reaches its peak mass, which is mostly influenced by genetics. In particular, genetic factors play a significant role in the body’s absorption of vitamin D. A person may be more susceptible to developing osteoporosis if their vitamin D absorption is poorer, which could potentially affect their ability to grow bones.
- Menopause: Lower levels of estrogen have an impact on the bone remodeling process and speed up the pace of bone loss as the body’s sex hormones alter throughout menopause, resulting in diminished bone strength and an increased risk of fracture.
- Menstrual history: A slightly increased risk for osteoporosis can result from light menstruation throughout life and/or an early menopause.
- Low testosterone: Osteoporosis can result from low testosterone levels in men through affecting bone development.
- Race: Asian and Caucasian women are more likely to get osteoporosis. 1 Although women of other races are less likely to be at risk, screening is nevertheless suggested if they are older than 65 or have any other risk factors.
Recognizing the Symptoms
Osteoporosis is often referred to as a silent disease since it does not typically manifest with noticeable symptoms like other health conditions.
No specific signals indicate its presence.
The primary indicator usually occurs when a bone breaks unexpectedly, particularly following a minor incident that normally wouldn’t cause harm.
Although osteoporosis doesn’t directly produce symptoms, some subtle changes may hint at weakening bones.
These include:
- Losing height
- Alterations in posture
- Potential shortness of breath due to compressed spinal discs impacting lung capacity
- Lower back pain in the lumbar spine
Detecting such changes by yourself can be challenging; you might observe variations in body structure, height, or posture more readily.
While it’s common to see older adults “shrinking” with age, this could signify the need to consult your doctor for a bone density assessment.
How is Osteoporosis Diagnosed?
When diagnosing osteoporosis, a doctor usually performs Bone Density Test – an imaging procedure – that evaluates the strength of the bones.
This test uses X-rays to asses the levels of calcium and other important minerals that are present in the bones.
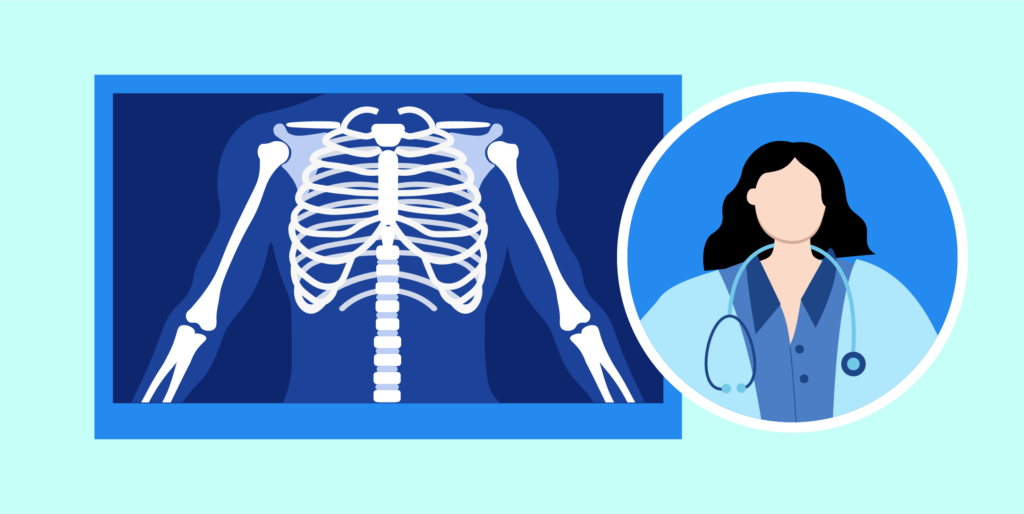
Healthcare experts use the terms like DEXA scan, DXA scan, or bone density scan, to mean bone density test.
The procedure is done by using extremely low levels of X-rays which assesses the bone density and mineral content.
As an outpatient procedure, the patient can go home immediately after the test without any hospitalization needed.
Bone Density Tests are recommended at least once a year for individuals with a history of osteoporosis in the family, those who are over 50 years old, or those already diagnosed with Osteopenia.
Early detection of osteoporosis is critical for preventing fractures.
Management and Treatment of Osteoporosis
Osteoporosis management requires a multifaceted approach which involves prevention of fractures, reduces bone loss and increases bone strength.
While there is no definitive cure, several strategies can effectively manage the condition:

Medications and Supplements
Healthcare providers may prescribe the drugs to enhance the bone density and to reduce the risk of fracture.
Medications include Bisphosphonates, HRT, Denosumab, SERMs, and Calcitonin.
Adequate calcium and vitamin D intake are key in maintaining healthy bones.
Supplements are suggested to ensure people do not lack needed nutrients each day.
Lifestyle Modifications
It is important to adopt a bone-friendly lifestyle.
Weight-bearing and muscle-strengthening exercises are done on a regular basis to ensure that bone mass is maintained.
It is also important to quit smoking, control alcohol consumption, and eat a balanced diet rich in calcium and vitamin D in order to have healthy bones.

Monitoring and Follow-Up
Monitoring through Bone Density Test and check-up with your doctor at regular intervals can determine the progression of osteoporosis and the effectiveness of the treatment.
Changes to the treatment plan can be made in response to the assessment.
Fall Prevention
Because of the increased risk of fractures in osteoporosis, fall prevention measures become very important.
This encompasses getting rid of home-tripping hazards, optimizing light fixtures, and providing assistive devices if these are needed.
Educational Support
The education and support offered to people with osteoporosis help them to better comprehend the condition, adhere to treatment plans, and make needed lifestyle changes for better bone development.
Osteoporosis Prevention
Preventing osteoporosis involves a comprehensive approach centered on fostering and sustaining robust bone health.

- Vital strategies for osteoporosis prevention encompass dietary modifications, emphasizing a balanced diet rich in calcium and vitamin D to fortify bones.
- Regular engagement in weight-bearing and muscle-strengthening exercises such as walking, jogging, weightlifting, and yoga is crucial to maintaining bone density and strength.
- Avoiding tobacco products and limiting alcohol consumption play pivotal roles in shielding bones from weakening.
- Bone Density Screenings allow for the early detection of bone loss and osteoporosis, particularly beneficial for individuals with predisposing factors.
- In certain cases, medical interventions like medications and supplements are prescribed to boost bone density and minimize fracture risks.
By adopting a holistic approach that integrates healthy lifestyle choices, consistent physical activity, and medical guidance, individuals can significantly diminish the likelihood of osteoporosis development, uphold bone vitality, and enhance overall quality of life for the long term.
Outlook (Prognosis)
The prognosis for individuals diagnosed with osteoporosis hinges on various factors, including timely intervention, adherence to treatment plans, and lifestyle adjustments.
While osteoporosis is a chronic condition with no definitive cure, proactive management strategies can significantly impact outcomes and overall well-being.
Early detection followed by appropriate treatment can help slow bone weakening.
Through a combination of medication, supplements, and therapies – individuals can enhance bone density and mitigate fracture risks.
Embracing a bone-friendly lifestyle encompassing regular exercise and a nutrient-rich diet are vital for managing osteoporosis effectively.
By staying engaged in treatment plans, making lifestyle modifications, and prioritizing preventive care, individuals with osteoporosis can expect an improved prognosis and enhanced quality of life.
Conclusion
In summary, osteoporosis prevention is a holistic approach which highlights the value of preventive actions to ensure bone strength and fracture risk reduction.
Bone Density Screenings and medication & supplements intake are additional steps to early detection and management of bone loss.
The holistic approach that includes healthy lifestyle choices, regular physical activity, and working with the healthcare providers lays the ground for a successful osteoporosis prevention.

