Spinal fractures are common, and they include compression fractures which occur when the vertebral bones compress or collapse.
Osteoporosis, trauma, and other medical issues could also trigger these fractures.
Chronic pain, loss of height, and decreased quality of life may result from compression fractures.
It is vital to comprehend what causes, symptoms, and treatment options exist for compression fracture in order to make an early diagnosis and appropriate management.
This article is going to take you through the world of compression fractures, highlighting their causes, symptoms, and treatments options.
This is a broad guide that caters to individuals who either suffered a compression fracture or seek information for their beloved ones experiencing the same.
What is Spinal Compression Fractures?
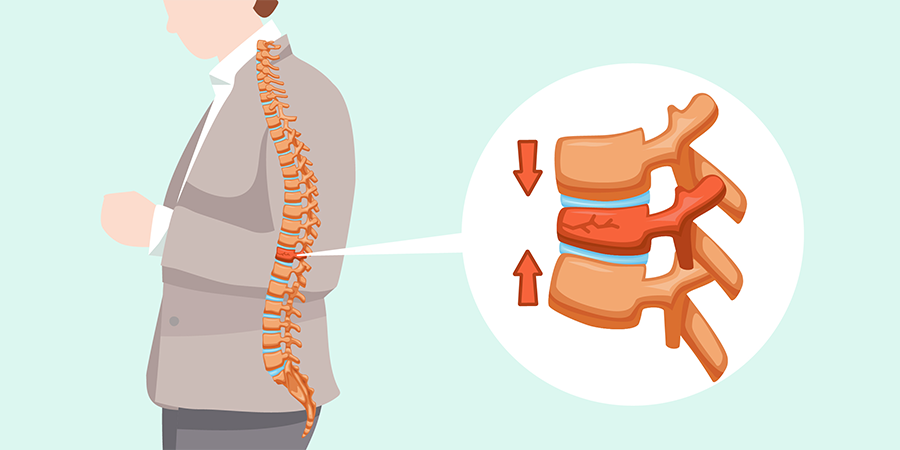
Compression fractures are small breaks or cracks in the vertebrae (the bones that make up your spinal column).
The breaks happen in the vertebral body, which is the thick, rounded part on the front of each vertebra.
Fractures in the bone cause the spine to weaken and collapse. Over time, these fractures affect posture.
The spine curves forward and the person looks “hunched over” (kyphosis).
Most compression fracture occurs in thoracic middle region, mostly lower thoracic region.
Healthcare providers may refer to them as Vertebral Compression Fractures (VCF).
Although Osteoporosis is a common cause, these fractures can also arise from trauma like a road traffic accident or even tumors of the spine.
Healthcare providers treat vertebral compression fractures through use of drugs and back braces that are specifically designed for the purpose.
At times, it becomes necessary to strengthen some of the vertebrae and stabilize the spinal column through a minimally invasive procedure.
The all-inclusive solution serves for relieving pain and improving the state of the patients suffering from the compression fractures.
How common are Compression Fractures?
The rate of compression fractures is extremely high; around 1 million cases annually in the United States alone.
These are the fracture known as the pathological factures which primarily affects in old women with osteoporosis which is the medical term for the weakening of the bone resulting in breakage at the weak points.
Nonetheless, compression fractures occur occasionally among elderly men as well.
Approximately one fourth of women aged 50 years or more will sustain at least one vertebral compression fracture and this risk is further accentuated following menopause.
Moreover, more than two in five people aged 80 years and above have experienced compression fracture at some moment in time.
These figures clearly demonstrate that compression fractures are a huge problem mostly among the older people.
Causes of Spinal Compression Fractures
Spinal compression fractures typically occur when the vertebral body, the block-like structure that forms the spine, collapses or becomes compressed.
The fractures result from severe osteoporosis characterized by fragile bones, which may arise from simple daily activities such as stepping out of the shower, forceful sneezing, or even lifting a light object.
Spinal compression fractures are usually caused by greater force or trauma such as falling, or even an attempt to lift heavy objects in those individuals suffering from the moderate osteoporotic condition.
- Out of all of the fractures, Spinal compression fractures are the most common ones seen in the patients suffering from osteoporosis.
- It can manifest themselves in over 1 million individuals annually.
- Approximately 25% of these postmenopausal women in the US experience these fractures and it has been proven these fractures occur more as a woman ages, with approximately 40% of females aged 80+.
- Spinal compression fractures are a common issue in older women but should not be ignored among older persons of both sexes.
- People who suffer a single spinal compression fracture have a five times higher chance of experiencing a recurrent spinal compression fracture.
Sometimes, it does not present any or very minimal symptoms, but the possibility of having additional spinal compression fractures remains high.
The main cause of spinal compression fracture in people who have healthy spines is usually severe trauma resulting from car accidents, sports injuries, or hard falls.
If there is no history of trauma in a patient who is below 55 years old and only with minimum trauma, then consider metastatic tumors as the possible cause.
This type of cancer commonly spreads through the bones of the spine. This may cause deterioration and breakdown of the affected vertebra leading to a spinal compression fracture.
Recognizing the Symptoms
Sudden and acute back pain can be symptomatic of a compression fracture.
However, not all fractures are accompanied by immediate symptoms. In other cases, a fracture could be found during an X-ray which has been carried out for different purposes.
As a compression fracture progresses and affects the vertebrae, you may experience the following symptoms:
- Gradually worsening back pain: This is because the pain gets worse when standing up and better when lying down on your back.
- Decreased height: Over a period, the bones will keep becoming smaller causing the height loss.
- Stooped-over posture: When affected by the vertebra, a forward-leaning or stooped posture, also called as kyphosis, may develop.
- Numbness or tingling: The nerve-related symptoms of numbness or a tingling sensation could result from the trauma leading to the fracture or compression and impairment of the nerve.
- Weak muscles and walking difficulties: The muscles that support the spine can become weakened, resulting in problems standing and walking straight.
Apart from fracture, bowel or bladder control may be interfered due to nerve damage.
However, if you experience any of these symptoms or suspect to have a compression fracture then you should visit your health practitioner for detailed assessment and management.
Physical Examination
Following the collection of your medical history, a physical examination will be conducted by the physician to investigate the potential causes of your pain and determine the underlying problem.
The specific areas of your body to be examined will depend on the location of your pain, such as the neck, lower back, arms, or legs.
It’s worth noting that neurological issues are rare, except for younger patients who have experienced severe trauma like a car crash.
If a compression fracture is suspected, the doctor will perform tests to identify point tenderness near specific vertebrae.
By assessing these tender areas, the doctor can narrow down the source of your pain.
To confirm the presence of a fracture, an X-ray of the spine is typically ordered.
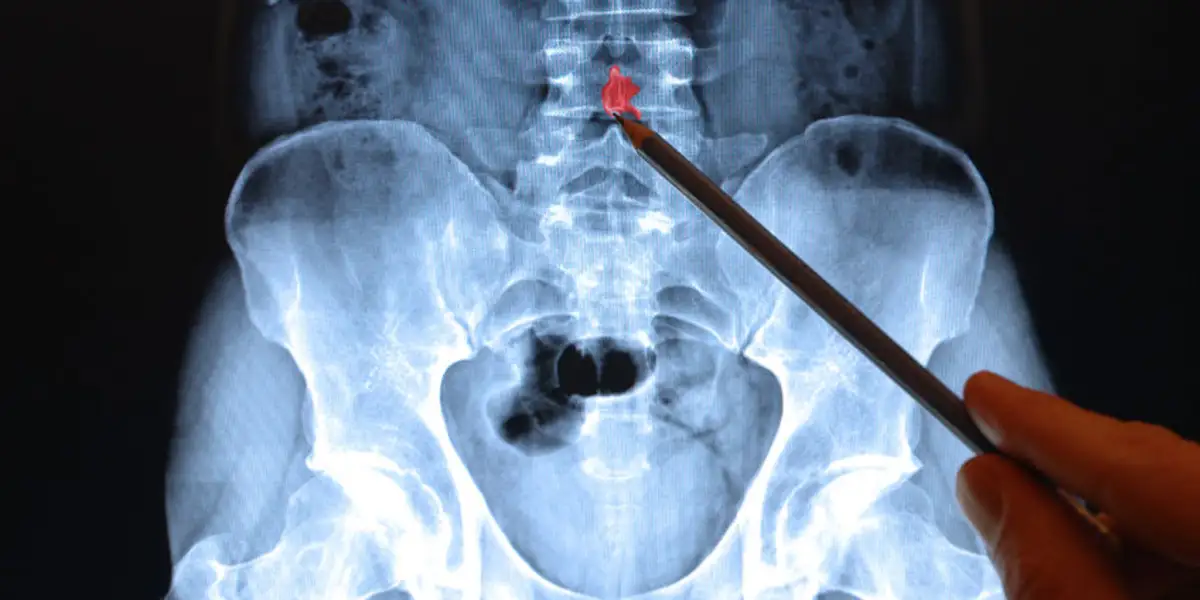
This painless procedure uses radioactive substances to capture images of the bones.
X-rays primarily visualize bones and provide limited information about soft tissues.
Therefore, X-rays are an integral part of diagnosing fractures.
If a fracture is presumed, a CAT scan may be recommended to assess its stability.
A CT scan is similar to both an MRI and a regular X-ray, as it can provide images of bones and soft tissues.

It produces cross-sectional images by taking “slices” of the spine, allowing for separate examination of each section.
This scan is particularly useful in evaluating the stability of a compression fracture and determining if there is any risk to the nerves.
A neurological examination will also be conducted to assess your neurological responses, including reflexes, muscle function, and sensory perception.
Abnormalities identified during this examination can indicate nerve damage.
The nerves of the spinal cord transmit messages from the brain to the rest of the body, so any spinal nerve damage may affect your body movement and neurological responses.
If there is a suspicion of nerve involvement in the fracture or uncertainty about the cause of pain, an MRI might be recommended.
Unlike X-rays, an MRI does not involve radiation. It utilizes magnetic and radio waves to generate computer-generated images.
An MRI can penetrate multiple layers of the spine, providing detailed information about soft tissues, such as nerves and ligaments.
A nuclear bone scan may also be ordered as a diagnostic test.
This scan helps determine the age of a fracture.
If the fracture is old and there is evidence of other healed fractures, it may indicate osteoporosis (a condition characterized by bone thinning) as the underlying cause.
This is particularly important for older patients, especially women.
In such cases, treatment for the fracture will include preventive measures to minimize the risk of future vertebral fractures.
This treatment may involve calcium supplements, increased vitamin D intake, weight-bearing exercises, and hormone replacement therapy for women.
Management and Treatment
Treating spinal compression fractures involves both pain management and addressing the underlying cause.
The following treatment options are commonly considered:
- Pain Medication: Over-the-counter pain relievers or prescribed medications can help alleviate discomfort associated with spinal compression fractures.
- Bracing: Wearing a brace or corset can support the spine and provide stability, reducing pain and allowing for healing.
- Rest and Activity Modification: Limiting physical activity and avoiding strenuous exercises that strain the spine can aid in pain management and promote healing.
- Vertebroplasty and Kyphoplasty: These minimally invasive procedures involve injecting medical-grade cement into the fractured vertebra, stabilizing it and relieving pain.
- Physical Therapy: Specific exercises and stretches prescribed by a physical therapist can help strengthen the back muscles, improve flexibility, and support the healing process.
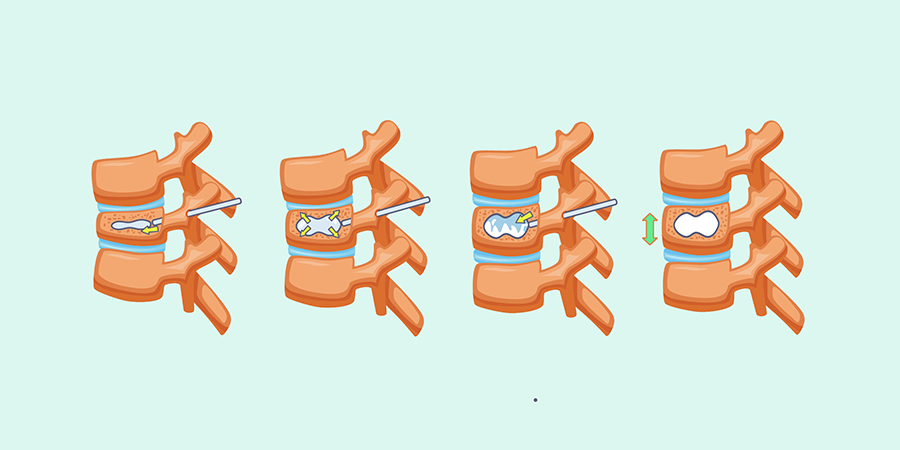
Kyphoplasty is a minimally invasive surgical procedure used primarily to treat spinal compression fractures.
It is often performed on patients with osteoporosis or those who have experienced trauma to the spine resulting in vertebral fractures.
The goal of kyphoplasty is to relieve pain, stabilize the fractured vertebra, and restore vertebral height.
During the kyphoplasty procedure, the patient is usually under local or general anesthesia. Here is an overview of the steps involved:
- Patient positioning: The patient is positioned face down on the operating table to allow access to the spine.
- Guidewire insertion: Under X-ray guidance, the surgeon inserts a needle into the fractured vertebra through a small incision in the back. A guidewire is then passed through the needle, creating a pathway for subsequent instrument placement.
- Balloon insertion and inflation: A specialized balloon is threaded over the guidewire and positioned within the collapsed vertebra. The balloon is carefully inflated to create a void or cavity in the vertebral body, restoring its height and correcting the deformity.
- Cement injection: Once the balloon is deflated and removed, the void created is filled with bone cement (a medical-grade material similar to epoxy). The cement is inserted into the vertebral body through the same access point used for the balloon.
- Cement hardening: The injected cement quickly hardens, stabilizing the fractured vertebra and providing structural support. This helps to relieve pain and prevent further collapse of the spine.
The entire kyphoplasty procedure typically takes about one hour per treated vertebra.
Patients usually experience immediate pain relief following the procedure and are able to resume light activities within a few days.
However, it is essential to follow the surgeon’s post-operative instructions regarding physical activity and rehabilitation to ensure proper healing.
It’s worth noting that kyphoplasty is different from vertebroplasty, another minimally invasive procedure used to treat spinal compression fractures.
While both procedures involve injecting bone cement into the vertebra, kyphoplasty also includes the use of a balloon to create a cavity and restore vertebral body height.
Vertebroplasty is a treatment option for vertebral compression fractures where a cement-like material is injected into the fractured vertebra.
While it can provide relief for patients, recent studies consistently show that kyphoplasty, a similar procedure with added benefits, is superior in saving lives compared to vertebroplasty.
Kyphoplasty has shown high success rates in relieving pain, improving mobility, and enhancing the overall quality of life for patients with spinal compression fractures.
However, like any medical procedure, it carries potential risks and complications, which should be discussed in detail with a qualified healthcare professional before making any treatment decisions.
Outlook (Prognosis)
In most cases, compression fractures resulting from injuries typically heal within 8 to 10 weeks with rest, the use of a brace, and pain medication.
However, if surgery was required, the recovery period may be significantly longer.
It’s important to note that some loss of height and increased spinal curvature may occur during the healing process.
Compression fractures caused by osteoporosis often become less painful with rest and pain medication.
However, certain fractures can lead to long-term chronic pain and disability.
Medications aimed at treating osteoporosis can help prevent future fractures.
However, they cannot reverse the damage that has already occurred.
When compression fractures are caused by tumors, the prognosis depends on the specific type of tumor involved.
Tumors that affect the spine can include breast cancer, lung cancer, lymphoma, prostate cancer, multiple myeloma, and hemangioma.
Possible Complications:
- Failure of bones to fuse properly after surgery
- Development of a humpback deformity
- Compression of the spinal cord or nerve roots, leading to potential neurological symptoms.
Remember, once you get one Compression Fracture, your risk for getting a second goes up 5X (500%).
If that sounds bad, by the second Compression Fracture, that risk increases to 9-12X – and by the third fracture, that’s mind-boggling 72X (7,200%) increased risk.
So for patients with more than one fracture it’s less of a question of IF and more of a question of WHEN.
Those are statistics from a large study. Just likely any other statistic, for an individual patient, it’s hard to quantify the risk.
Some patients do not get another fracture for 5 or more years – and others have 10 fractures in the first year.
Preventing Spinal Compression Fractures
While complete prevention may not always be possible, certain measures can help reduce the risk of spinal compression fractures:
- Maintain Bone Health: Adopt a diet rich in calcium and vitamin D, engage in weight-bearing exercises regularly, and avoid habits that weaken bones, such as smoking or excessive alcohol consumption.
- Fall Prevention: Take precautions to minimize the risk of falls, such as ensuring adequate lighting, removing tripping hazards, and using assistive devices when necessary.
- Regular Check-ups: Regular bone density screenings can help detect osteoporosis early, allowing for early intervention and preventive measures.
Conclusion
Spinal compression fractures can significantly impact an individual’s mobility and overall well-being.
Understanding the causes, recognizing the symptoms, and exploring the available treatment options is vital for managing this condition effectively.
By adopting preventive measures and seeking timely medical care, individuals at risk can take proactive steps toward minimizing the impact of spinal compression fractures and maintaining their spinal health.
Remember, if you suspect you may have a spinal compression fracture or are experiencing persistent back pain, it is crucial to consult with a medical professional to receive an accurate diagnosis and appropriate treatment.
Reference List
- https://my.clevelandclinic.org/health/diseases/21950-compression-fractures
- https://www.cedars-sinai.org/health-library/diseases-and-conditions/c/compression-fracture.html
- https://www.umms.org/ummc/health-services/orthopedics/services/spine/patient-guides/lumbar-compression-fractures
- https://www.pennmedicine.org/for-patients-and-visitors/patient-information/conditions-treated-a-to-z/compression-fracture
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/compression-fractures
- https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Vertebral-Compression-Fractures

